BACKGROUND
A number of studies have shown that mental health issues are a substantial problem in numerous countries (Alonso et al., 2004; Bobak et al., 2006; Kużel et al., 2015), including Poland (Kiejna et al., 2015a). European epidemiological studies indicate that over 11% of the European Union’s adult population suffers from depression (Kużel et al., 2015). The World Health Organization (WHO) reported that about 350 million people are suffering from depression worldwide and it is the second cause of disability in the world (Murawiec & Wierzbiński, 2016). For example, the prevalence of major depressive disorder was estimated at 9.8% in Israel (n = 4859), at 9.9% in Italy (n = 4712), at 9.9% in Germany (n = 3555), at 10.6% in Spain (n = 5473), at 14.1% in Belgium (n = 2419), at 17.9% in the Netherlands (n = 2372) and at 21.0% in France (n = 2894; Alonso et al., 2004). Similarly to the global trend, the number of people with depression is growing in Poland and currently stands at 1.8 million (WHO, 2017). In a cross-sectional study in Poland, the prevalence of depressive symptoms was around 21% in men and 40% in women (Bobak et al., 2006). Epidemiological reports estimate that signs of generalized anxiety disorder occur in approximately 1% of the population. In Poland, the most frequently diagnosed disorders were panic attacks (6.2%), specific phobias (3.4%), and major depressive disorder (3.2%; Kiejna et al., 2015b). As anxiety and depression become more prevalent (Kazmi et al., 2020; Liu et al., 2020; Mazza et al., 2020; Moghanibashi-Mansourieh, 2020; Shevlin et al., 2020; Ueda et al., 2020; Wang et al., 2021) it is important to understand numerous risk factors that may increase the likelihood of mental health deterioration. Depression and anxiety have been studied in the context of stress, quality of life, and health outcomes (Angermeyer et al., 2002; Eisner et al., 2010; Vignola et al., 2008). In spite of studies confirming the prevalence of depression and anxiety and their co-occurrence with physical disorders (Scott et al., 2007) the question of dispositional and situational factors affecting the mental health outcomes remains salient. Therefore in the current research, we wanted to corroborate previous findings of the direct relations between generalized self-efficacy and perfectionism with anxiety and depression alongside testing hypothetical indirect relations between dispositional traits and mental health outcomes via health behaviors.
PERFECTIONISM AND HEALTH
Clinical perfectionism is a tendency to set very high standards for oneself, which are related to high concerns about failure and also elevated levels of negative emotions in the situation of failure (Hewitt et al., 2003). It can also be described as a discrepancy between a person’s abilities and the requirements they place on themselves (Hewitt et al., 2003). Hewitt and Flett (1991) suggested that perfectionism is a three-dimensional construct, comprising self-oriented perfectionism, socially prescribed perfectionism, and other-oriented perfectionism. Self-oriented perfectionism is the setting of high standards for oneself and an excessive motivation to attain perfection of the self. Socially prescribed perfectionism characterizes the beliefs that others are demanding perfectionistic standards and shows strong associations with depression. Other-oriented perfectionism is related to demanding these standards and perfection from other people.
The model of clinical perfectionism by Shafran et al. (2002) assumes a strong dependency of self-esteem on the pursuit of personally imposed standards in at least one domain of life, even if this may have negative consequences. Hamachek (1978) distinguished two types of perfectionists: healthy (adaptive) and unhealthy (maladaptive). The first is characterized by more flexible action, acceptance of discrepancies between their level of performance and their standards, and thus acceptance of possible mistakes. Unhealthy perfectionism is characterized by very high standards set for oneself, a feeling that what is done is never good enough, an intense fear of failure, and a lack of satisfaction with one’s actions.
Studies demonstrate that perfectionism is related to health behavior. For example, maladaptive perfectionism is associated with a reduced level of involvement in preventive health behaviors, whereas adaptive perfectionism is associated with a higher level of commitment to preventive health behaviors. Also, maladaptive perfectionism is associated with higher levels of psychological distress (Williams & Cropley, 2014). Furthermore, socially prescribed perfectionism was associated with higher negative affect, and fewer health-promoting behaviors (Sirois & Molnar, 2016).
Moreover, maladaptive perfectionism can pose risk for the development of psychopathologies, such as depressive and anxiety symptoms, which are known to have an effect on health behavior and physical health (Sirois & Molnar, 2016). Wheeler et al. (2011) found a connection between maladaptive perfectionism and social anxiety disorder (SAD), panic disorder, and obsessive-compulsive disorder (OCD). Furthermore, Dunkley et al. (2000) found that the relationship between evaluative concerns, perfectionism and distress was mediated by avoidant coping, which is known to exacerbate anxiety symptoms (Blalock & Joiner, 2000; also see: Weiner & Carton, 2012). Maladaptive perfectionism is associated with depression as well (Chang, 2000; Hewitt & Flett, 1991; Kawamura et al., 2001; Sherry et al., 2015) and predicts increases in depressive symptomatology (Egan et al., 2011; Smith et al., 2017). For example, studies show that self-oriented perfectionism, which involves high self-criticism, is correlated strongly with increased rates of depression (Blatt, 1995). Another study, by McGrath et al. (2012), found that self-critical perfectionism is linked to depression bidirectionally, namely, persons high in self-critical perfectionism may find themselves entangled in a pattern where self-critical perfectionism both leads to, and results from, depressive symptoms.
SELF-EFFICACY AND HEALTH
Self-efficacy is understood as the conviction of an individual that he or she has the skills and resources to cope with adversity and thus to achieve goals (Bandura, 1994). A generalized sense of self-efficacy is an individual’s general belief in the effectiveness of coping with difficult situations and obstacles, reflecting the individual’s resources to help him or her cope with problems in various areas of life (Schwarzer & Jerusalem, 1995; see: Luszczynska et al., 2005b). Juczyński (2001) emphasizes that beliefs about effectiveness influence the assessment of the individual’s resources in stressful situations. The belief in one’s effectiveness is significantly related to one’s emotional state, thinking, motivation, and behavior. People with a high sense of self-efficacy choose difficult tasks more often and set themselves more demanding goals, which they consistently pursue. Additionally, a high self-efficacy level may facilitate coping with a threatening situation, by perceiving it as a situation that can be controlled.
According to the Health Action Process Approach (HAPA; Schwarzer et al., 2011), self-efficacy plays an important role in health behaviors. Health behaviors can be reactive, habitual, or intentional. The latter can be considered a result of objective knowledge about health. These activities are undertaken for health reasons or have a proven impact on health (Luszczynska, 2004). Juczyński (2001) specified categories of health behaviors, dividing them into healthy eating habits, preventive behaviors in the form of following doctors’ instructions and health-promoting education, health practices understood as everyday activities or habits related to sleep time, optimistic thinking, and attitude in the face of strong emotions, as well as coping with stress and everyday emotional tensions. The procedural Health Behavioral Model assumes two main stages of behavior change, the motivational phase preceding the action (formulation of intentions) and the implementation (volitional) phase (Schwarzer & Luszczynska, 2008). In the motivational phase, one’s effectiveness in initiating the process plays the most important role. Sense of self-efficacy influences the shape of intentions and formulation of an action plan. In the implementation phase, one’s effectiveness sustains the action and determines its further continuation despite possible difficulties (Luszczynska, 2004). Finally, when an individual ceases to act and returns to unfavorable health behaviors, the sense of one’s effectiveness may facilitate the resumption of behavioral change (Schwarzer & Luszczynska, 2008). People with a higher level of self-efficacy are more involved in health behaviors (Luszczynska et al., 2005b). Research by Baumgart et al. (2015) shows that there is a relationship between self-efficacy and health behaviors in terms of correct eating habits, preventive behaviors, positive mental attitudes, and health practices. According to Nguyen et al. (2020) the knowledge of health issues may be a protective factor against anxiety. Additionally, studies revealed that there is a significant negative relationship between generalized self-efficacy and depression (Luszczynska et al., 2005a) as well as anxiety (Endler et al., 2001).
THE CURRENT STUDY
The present study focused on examining the relationships between anxiety, depression, perfectionism, and self-efficacy jointly. While numerous studies confirm the existence of relations between those variables (including bidirectional ones), a comprehensive evaluation of their interrelations in one study is yet to be conducted. We wanted to replicate existing findings (Sirois & Molnar, 2016; Williams & Cropley, 2014) and broaden their scope by determining the role of dispositional traits (such as perfectionism and generalized self-efficacy) and health behaviors (explicitly preventive practices, and general health attitude represented by overall Health Behavior Inventory scores) in predicting anxiety and depression. We also wanted to examine possible indirect relations between perfectionism, self-efficacy and mental health outcomes, namely whether health behaviors mediate these relationships.
Based on previous findings (Blalock & Joiner, 2000; Blatt, 1995; Chang, 2000; Egan et al., 2011; Hewitt & Flett, 1991; Kawamura et al., 2001; Mc- Grath et al., 2012; Sherry et al., 2015; Smith et al., 2017; Weiner & Carton, 2012; Wheeler et al., 2011), we expected that participants who display higher levels of maladaptive perfectionism would be prone to experiencing more anxiety and depression symptoms (hypothesis 1). We assumed that high self-efficacy would be a protective factor against anxiety and depression (hypothesis 2) because participants who perceive themselves as having the skills and resources to cope would perceive any adversities as more manageable than those with low levels of selfefficacy. Furthermore, we predicted that self-efficacy and adaptive perfectionism would positively predict health behaviors (hypothesis 3). We also assumed that the relationship between perfectionism, generalized self-efficacy, and mental health symptoms (anxiety and depression) would be both direct and indirect (mediated by health behaviors and preventive practices, hypothesis 4).
PARTICIPANTS AND PROCEDURE
PROCEDURE
The required study sample was calculated with G*Power software (Faul et al., 2009). In order to detect an effect size of f2 = 0.1 with an error probability of α = 0.05 (power of 0.95) for multiple regression with 17 theoretically possible model parameters, a study sample of 305 participants would be sufficient. The number of complete datasets we decided to obtain was larger since data sets usually require screening, which results in a sample size reduction.
Data collection procedures meet the ethical standards outlined in the Helsinki Declaration of 1975 as revised in 2000 and were approved by the institutional ethics committee. All participants consented to fill in the questionnaires and were able to withdraw from the study at any point. The initial sample consisted of 320 participants (69.6% women). It is worth noting that the data were gathered during the ongoing COVID-19 pandemic, although at the time all the pandemic restrictions had been loosened.
The data were screened for automated and invalid responses before testing the hypotheses. Data from participants who completed the study in less than five minutes were excluded from the analysis. Then, we analyzed the data and eliminated unreliable responses (automated, repeated responses).
PARTICIPANTS
The total number of subjects qualified for the calculation stage was 295 participants (72.8% women). Participants ranged in age from 18 to 84 years (M = 28.16, SD = 9.41). One hundred twenty-five (42%) respondents were not currently in a relationship, while 170 (58%) reported being romantically involved. Of the participants, 6 (2%) reported primary education, 106 (36%) reported secondary education, and 183 (62%) reported higher education. Regarding the place of residence, 50 (17%) currently live in a village, 245 (83%) in a city.
The participants were invited to take part in the study via a social media message that included a brief description and a link to the survey. They were informed that their participation was voluntary and anonymous. After reading the instructions and providing informed consent, the participants completed a demographic survey and a series of questionnaires.
MEASURES
The following scales were used in the study: the Generalized Self-Efficacy Scale by Schwarzer and Jerusalem (1995) in Polish translation by Juczyński (2000); the Health Behavior Inventory developed by Juczyński (2001), the Questionnaire of Adaptive and Maladaptive Perfectionism by Szczucka (2010), the Hospital Anxiety and Depression Scale (HADS) by Zigmond and Snaith (1983) in the Polish translation by Majkowicz (2000). The reliability coefficients for the measures calculated from our sample are provided in Table 1.
Table 1
Pearson correlation matrix, descriptive statistics, and reliability coefficients
The Generalized Self-Efficacy Scale (GSES; Schwarzer & Jerusalem, 1995) is based on Bandura’s concept of effectiveness. It is a unidimensional construct comprising 10 statements concerning an individual’s general belief in the effectiveness of coping with difficult situations and obstacles. Participants refer to those statements on a scale from 1 (no) to 4 (yes). Sample items include “I always manage to solve difficult problems if I try hard enough”, “If someone opposes me, I can find the means and ways to get what I want”. The results range from 10 to 40 (the higher the score, the greater the sense of effectiveness). Reliability coefficients for different language versions of the scale range from .91 (Japanese version) to .78 (Greek version).
The Health Behavior Inventory (HBI; Juczyński, 2001) is based on Gochman’s theory of health behaviors, indicating that the formation of health behaviors results from beliefs, expectations, thought patterns, and emotions. The test consists of 24 statements, and respondents assess how frequently they engage in described health practices on a scale from 1 (almost never) to 5 (almost always). Sample items include “I eat a lot of vegetables and fruits”, “I prevent colds”. The reliability of the scale is satisfactory – with Cronbach’s α of .85. There are four subscales corresponding with four subtypes of health behavior: healthy eating habits, preventive behaviors, positive mental attitude, and health practices (Juczyński, 2001). For the purpose of the study, we report general scores of the HBI and preventive behaviors. The indicators of preventive behavior are: avoiding colds, having telephone numbers of the emergency services recorded, adhering to recommendations of medical examinations, reporting for medical examinations regularly, searching for information on disease avoidance, and understanding the determinants of health and disease.
The Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, 1983) is designed to study the level of state anxiety (White et al., 1999) and depression. The scale consists of 14 statements, 7 of which measure symptoms of anxiety (e.g. “Worrying thoughts go through my mind”; “I can sit at ease and feel relaxed”) and 7 measure symptoms of depression (e.g. “I can laugh and see the funny side of things”, “I can enjoy a good book or radio or TV program”). Participants refer to those statements on a 4-point scale that indicates a qualitative or a quantitative change in experienced symptoms. Results between 0 and 7 are within the norm, results between 8 and 10 are borderline results, indicating a decline in mental health, and results equal to or higher than 11 suggest a mental health disorder. Cronbach’s α for the HADS-Anxiety subscale in previous studies ranged from .68 to .93. Cronbach’s α for the HADS-Depression subscale ranged from .67 to .90 (Boxley et al., 2016).
The Adaptive and Maladaptive Perfectionism Questionnaire (KPAD; Szczucka, 2010). The KPAD questionnaire, designed to study perfectionism, consists of 35 statements. It examines two aspects of perfectionism – adaptive and maladaptive perfectionism. The subjects determine on a 7-degree scale (1 – I strongly disagree, 7 – I strongly agree) to what extent each statement is an accurate description of themselves (e.g. “What I do never seems to be good enough for me”, “To make a mistake is a total failure”). As reported by Szczucka (2010), the Maladaptive Perfectionism subscale has a Cronbach’s α reliability of .95 whereas the Adaptive Perfectionism subscale has a reliability of .89, therefore indicating good psychometric properties.
STATISTICAL ANALYSIS
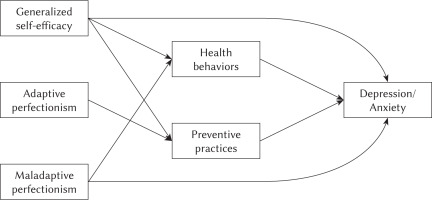
The analytical strategy for the study included variable distribution analysis in order to choose adequate subsequent statistical tests and to establish the prevalence of anxiety and depression symptoms among participants. The skewness and kurtosis for all variables were acceptable (< 1 for skewness, < 2 for kurtosis; George & Mallery, 2010), allowing the use of parametric tests. In the next step, the correlation analysis was conducted to establish linear relationships among variables. Finally, regression and path analyses were conducted to establish the direct and indirect effects of the independent variables on mental health outcomes. Upon conducting multiple regression analyses, the hypothesized paths in predicting anxiety and depression were developed (the proposed conceptual model is displayed in Figure1). The analyses were performed in Statistica 13.3 software (descriptive statistics, correlational and regression analyses) and in R-Studio using the lavaan function (path analysis).
RESULTS
We were interested in the prevalence of mental health outcomes both in itself and with regard to achieved variance in depression and anxiety in our sample. The HADS scale allows one to measure levels of depression and anxiety that meet dysfunction criteria. We found that 38.9% of the sample (115 participants) experienced anxiety levels that meet the criteria of anxiety disorders, and 19% (57 participants) could be qualified as overly anxious. 16.9% (50 participants) of the sample were experiencing depression symptoms that meet dysfunction criteria and an additional 18.6% (55 participants) experienced mild depressed mood symptoms. 14.9% (44 participants) experienced both depression and anxiety symptoms that meet the disorder criteria; thus a majority of the participants who scored high on the depression subscale experienced anxiety symptoms as well (44 out of 50). The analyses revealed a number of significant zero-order correlations between perfectionism, self-efficacy, health behaviors, and anxiety/depression symptoms (Table 1).
Adaptive perfectionism correlated significantly with health behaviors and with preventive practices (positive correlations) as well as with depression symptoms (negative correlations), but not with anxiety symptoms. Maladaptive perfectionism correlated significantly with both mental health outcomes (positively) and health behavior variables (negatively). Also, self-efficacy correlated negatively with mental health outcomes, and maladaptive perfectionism correlated positively with mental health outcomes.
In the next step, we conducted a series of multiple regression analyses to predict anxiety and depression based on perfectionism (adaptive and maladaptive), generalized self-efficacy, and health-related behaviors. The first set of analyses was designed to assess the role of generalized self-efficacy and perfectionism in predicting mental health outcomes. The second set of analyses aimed at verifying whether health behaviors significantly predict mental health outcomes. In the third set of analyses, we wanted to verify whether dispositional traits predict health behaviors. We conducted separate regression analyses (separating dispositional tendencies, health behaviors, and mental health outcomes) instead of including all variables into one model for two reasons. Firstly, we wanted to replicate previous findings (hypotheses 1-3), and secondly, we wanted to develop a model to be tested in the path analysis based on confirmed significant linear relations among the variables. The detailed results of the regression analyses are available in the Supplementary Material.
The regression analyses showed that people who are high in adaptive perfectionism are more likely to engage in preventive practices compared to those who are low in adaptive perfectionism (partially corroborating hypothesis 3). People who reveal high levels of maladaptive perfectionism are more prone to experiencing anxiety and depression symptoms (as predicted in hypothesis 1) and engage in general health-promoting behaviors to a lesser degree. Furthermore, those who exhibit higher levels of self-efficacy are less likely to experience depression and anxiety symptoms and are more likely to engage in practices conducive to health (in accordance with hypotheses 2 and 3).
Since the path analysis allows one to simultaneously test numerous linear relationships among variables with an additional estimation of model fit, there is an advantage of path analysis in comparison with regression models (Singh & Wilkes, 1996). In the current study we conducted two path analyses: in predicting anxiety and in predicting depression. The path analyses included both the direct and indirect effects of dispositional variables and health behaviors on mental health outcomes. The assumed relationships among the variables were based on previous findings and precisely established using empirical findings from our regression analyses (Figure 1). For example, the direct effect of adaptive perfectionism on mental health outcomes was not grounded in previous findings and was insignificant in our regression analyses; therefore it was not included in the tested path models.
Figure 1
Hypothesized path model in predicting depression and anxiety based on generalized self-efficacy, perfectionism, and health behaviors
The path model for predicting anxiety (Figure 2) via direct and indirect paths was estimated using the maximum likelihood method using 1000 bootstrap draws. According to fit analysis, the model accounted for 47.5% of the variance in anxiety and was proven to fit with the data (CFI = .99, TLI = .99, SRMS = .02, RMSEA = .046). All the identified paths turned out to be statistically significant in the specified model. The path estimates (Table 2) suggest that the strongest direct predictor of anxiety was the preventive practices variable, followed by generalized self-efficacy and total health behaviors. Among the indirect effects, the interaction of generalized self-efficacy and total health behaviors was the strongest predictor of anxiety; it was also stronger in comparison with maladaptive perfectionism as a direct predictor.
Figure 2
Path analysis model of associations between dispositional traits, health behaviors and anxiety
Note. The path analysis shows direct and indirect associations among dispositional traits (generalized self-efficacy, maladaptive and adaptive perfectionism) and anxiety. Indirect paths are mediated by health behaviors and preventive practices. **p < .01, ***p < .001.
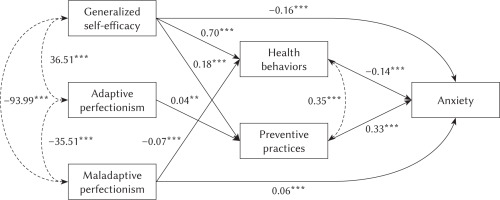
Table 2
Direct and indirect path estimates in predicting anxiety
The path model for predicting depression (Figure 3) was estimated using the same parameters. According to the model fit analysis, the variables accounted for 58.1% of the variance in depression symptoms. The model was proven to fit with the data as well (CFI = .99, TLI = .97, SRMS = .02, RMSEA = .063).
Figure 3
Path analysis model of associations between dispositional traits, health behaviors and depression
Note. The path analysis shows direct and indirect associations among dispositional traits (generalized self-efficacy, maladaptive and adaptive perfectionism) and depression. Indirect paths are mediated by health behaviors and preventive practices. **p < .01, ***p < .001.
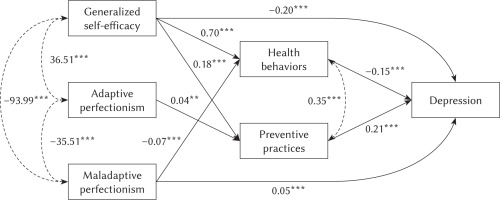
All the identified paths turned out to be statistically significant in the specified model. According to the path estimates (Table 3), preventive practices and generalized self-efficacy were the two strongest direct predictors of depression, followed by total health behaviors. Among the indirect effects, the interaction of generalized self-efficacy and total health behaviors was the strongest predictor of depression. Maladaptive perfectionism as a direct predictor and other indirect effects were found to predict depression to a lesser degree.
Table 3
Direct and indirect path estimates in predicting depression
DISCUSSION
The results of our research replicate previous findings regarding the negative correlation between maladaptive perfectionism and health behavior, as previously observed by Williams and Cropley (2014), and its role in predicting anxiety and depression (Chang, 2000; Kawamura et al., 2001; Sherry et al., 2015). Additionally, the current research revealed a negative correlation between generalized self-efficacy and mental health outcomes. The finding that people with a higher level of self-efficacy tend to become more involved in protecting their health by various means is consistent with the previous findings (Baumgart et al., 2015; Luszczynska et al., 2005b). Thus, dispositional beliefs in the effectiveness of coping with difficult situations and obstacles have proven to be a protective factor against depression and anxiety.
The predictive power of generalized self-efficacy may be rooted in its motivational function, as according to Bandura (1994) the level of self-efficacy can strengthen or hinder the motivation to change certain behaviors. It may also be important in terms of engaging in health behavior. Self-efficacy beliefs, understood according to Bandura’s model, can be significantly related to the initial motivation and a resulting decision to change health practices. The strongest relationship between self-efficacy and health behaviors in our study could be explained by the fact that people with a high sense of self-efficacy are less likely to experience fear of failure and to procrastinate. These emotional and motivational tendencies could favor actions related to health. On the other hand, fear of failure experienced by people high in maladaptive perfectionism (Jahani et al., 2018) may prevent them from properly engaging in actions aimed at health (e.g. the need to find the best physician, medication or health routine may postpone actual engagement in change).
Interestingly, in our path model generalized self-efficacy was the only significant predictor of health behaviors and preventive practices (in spite of significant zero-order correlations between both measures of perfectionism and health-related variables). Also, health practices were a stronger predictor of mental health outcomes than preventive practices in regression analyses, whereas in the overall path model, generalized self-efficacy (negatively) and preventive practices (positively) predicted mental health outcomes the most strongly, followed by health behaviors and the interaction of generalized self-efficacy and health behaviors (as negative predictors). These findings support the assumption that unique effects can be detected when related personality traits are controlled for in more complex models. Although the effect size of the detected estimates is small, the detected patterns can provide insight into the mechanism of the development of mental health pathologies.
The results indicated that the use of preventive practices positively predicted both anxiety and depression in the tested model. Presumably, people high in adaptive perfectionism and in sense of self-efficacy are more likely to undertake preventive strategies such as adherence to medical recommendations, seeking information on disease avoidance, etc. Those behaviors may function as protective means aimed at reducing the severity of illness-related anxiety, which as a consequence could perpetuate the problem of experiencing anxiety (Blalock & Joiner, 2000; Mowrer, 1960). On the other hand, the relationship between preventive practices and depression in the model we tested may be interpreted in terms of the effects of psychological stress on depression in the current context (an ongoing, chronic stressor of the pandemic). Experiencing stress may involve the loss of immune resources and exhaustion, and an individual’s maintenance of health depends on the amount of resources they have (Hobfoll, 1989). Engagement in preventive actions (as a coping strategy) may lead to the loss of resources protecting against the stage of exhaustion (Selye, 1956). High engagement in preventive practices (displayed by people high in generalized self-efficacy and adaptive perfectionism) may lead to a greater loss of resources and in turn make them more likely to experience deterioration of their mental health. Contrarily, a more balanced approach towards health, represented by the total score of health practices, seems to be related to diminished proneness to depression and anxiety.
LIMITATIONS
Several factors may limit our conclusions. The sample included a majority of women (69%), which might limit the possibility to generalize the results. The study was only cross-sectional, and was based on correlational data; therefore any causal inferences remain theoretical, and the data only support them. The procedure of the study relied on volunteers, and therefore its generalizability should be carefully reviewed. It is also worth noting that people may engage in other protective factors, not taken into account in this study. One of them could be the level of social support. For example, Teleki et al. (2022) suggest that social support can be a crucial component in facilitating healthy dietary behavior. Furthermore, our study relies on a path model formulated based on previous studies and regression analyses. In future studies other models could be developed and compared. Additionally, our study was conducted in a specific time (mid-COVID-19 pandemic). Yet we believe that the fact that our findings are consistent with previous reports suggests that the patterns our study revealed may be universal.
As for the analytical strategy, we are aware of the shortcomings of path analysis and of the advantages of the use of latent path models (Coffman & MacCallum, 2005). In path analysis the presence of measurement error will result in a certain level of imprecision, which can be eliminated with the proper use of SEM modeling. Conducting SEM analysis was not possible due to the sample size not being sufficient for estimating a required number of parameters (which would increase if latent factor loadings had been included in the model). However, since the measurement error very often contributes to an underestimation of effects among variables (Coffman & MacCallum, 2005), we believe our results still provide valuable insight.
IMPLICATIONS AND FUTURE DIRECTIONS
These findings may indicate that to address the mental health crisis it would be beneficial to address dispositional tendencies, such as perfectionism or generalized self-efficacy, that may affect one’s attempts to change one’s health-related behaviors alongside psychoeducation about the importance of a holistic approach to health. According to Egan et al. (2015), perfectionistic tendencies can be modified through therapy, indicating that it is a malleable personality trait. Such interventions could improve the implementation of actions taken by a person, and have a significant impact on their physical and mental health. Behavior change attempts made by overly perfectionist people may be consistently viewed by them as not good enough, and therefore lower their motivation to undertake protective measures. Thus it is also important to address specific behaviors – broadening their scope of adopted health protective measures – and promote beliefs about the effectiveness of their actions. It therefore seems beneficial to support people in strengthening their sense of self-efficacy and help them reduce maladaptive perfectionistic tendencies, encouraging them at the same time to apply diverse means of maintaining health.
A therapist can use a variety of techniques in intervention and therapy, including cognitive-behavioral methods, which are effective in increasing self-efficacy and reducing the perfectionistic tendencies, including the associated black and white thinking (Shafran et al., 2002; Shafran et al., 2010). Positive changes in perceived self-efficacy have been linked to improved adaptive emotional and behavioral responding in the context of anxiety-provoking situations. The current study also provides support for the use of interventions aimed at developing flexible and multilateral health-promoting strategies. It may also be inferred that the reduction of avoidant coping (i.e. striving for a perfect health routine) might be beneficial in terms of anxiety and depression prevention.
As for future directions, the indirect effects of perfectionism and self-efficacy on mental health outcomes via health behaviors should be analyzed in studies with a longitudinal design. Also a replication of the current study on a larger sample and verifying the model using latent variables (SEM modelling) is highly recommended. Furthermore, it remains to be verified whether the proposed interventions based on addressing both dispositional tendencies and health-related strategies would lead to an improvement in participants’ mental health. An empirical verification of the practical application of our findings is needed.
As this was our first attempt to integrate dispositional tendencies’ and health behavior’s influence on mental health outcomes, we believe that the aim of the study has been achieved. By improving our understanding of complex interrelations between significant factors affecting mental health, more effective strategies to reduce the adverse psychological effects and psychiatric symptoms can be developed. As depression and anxiety are experienced by a growing number of people, evidence-based, targeted treatments seem increasingly important.
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Supplementary material is available on journal's website.